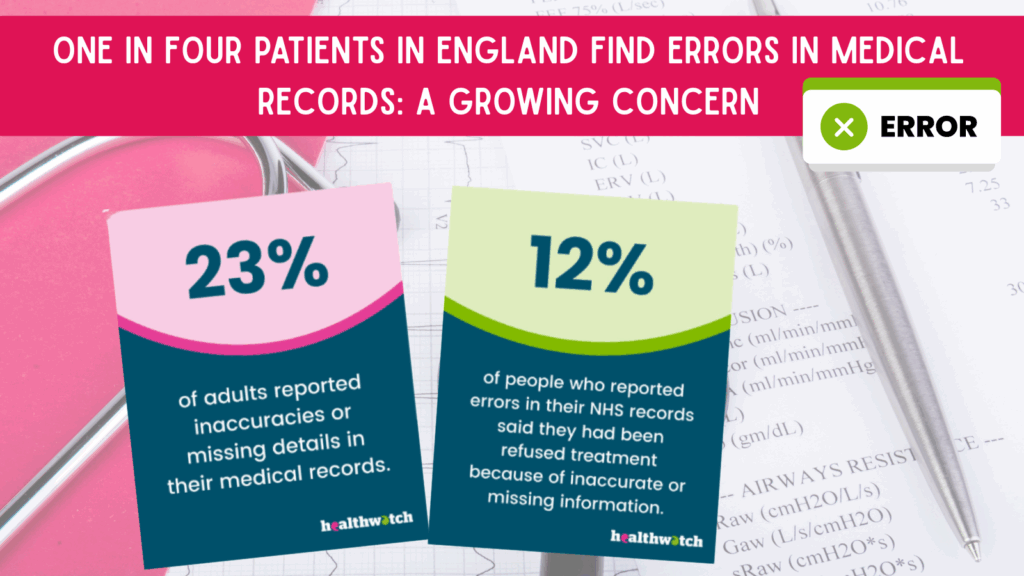
A recent report by Healthwatch England has revealed a startling statistic: nearly one in four patients in England (23%) have identified errors in their medical records, ranging from incorrect personal details to serious mistakes about diagnoses or treatments. Published on May 1, 2025, in The Guardian, the findings highlight systemic issues within the National Health Service (NHS) that could jeopardise patient safety and care quality. This article explores the scope of the problem, its implications, and what individuals can do to address inaccuracies in their medical records.
Additional Verification
A Healthwatch England survey of 1,800 adults, stated 409 respondents reported inaccuracies in their NHS medical records. The watchdog, tasked with championing patient experiences, emphasised that these errors have led to severe consequences, including patients being denied care or receiving inappropriate medications. (https://www.healthwatch.co.uk/blog/2025-05-01/extent-and-impact-inaccurate-nhs-patient-records)
BBC News (May 1, 2025): Reported that Healthwatch England’s survey found 23% of patients identified errors, such as wrong medications or false diagnoses, urging the NHS to prioritise accurate record-keeping before transitioning to a paperless system.
Multiple posts, including from @HealthwatchE and @radionewshub, echoed the 23% figure, with users sharing anecdotes of errors like incorrect Do Not Resuscitate (DNR) orders. While anecdotal, these align with the survey’s findings.
NHS England Patient Safety Reports (2024): While not directly tied to the 2025 survey, NHS incident reports from 2024 noted over 900 cases of potential patient harm linked to electronic record system errors at one trust, suggesting a broader issue with record accuracy.
Critical examination reveals no conflicting data, but the lack of longitudinal studies limits understanding of whether this issue has worsened over time.
The Scope of the Problem
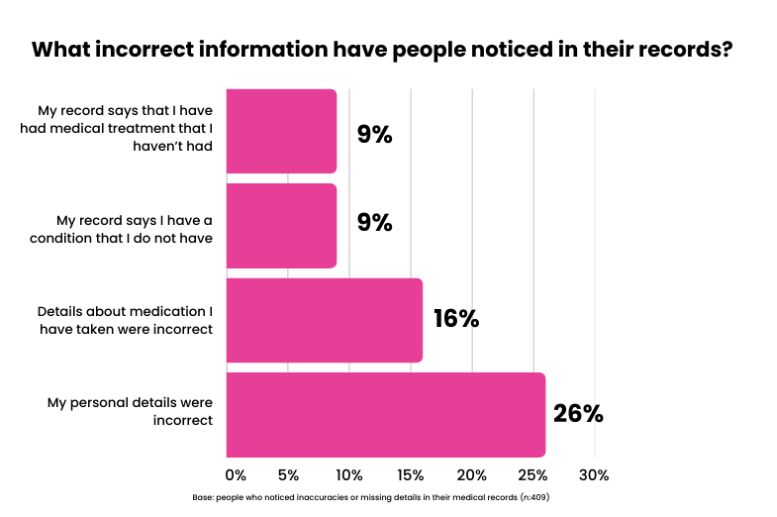
The errors identified range from minor administrative mistakes to critical clinical inaccuracies:
- Administrative Errors: Incorrect names, dates of birth, or contact details, which can lead to miscommunication or missed appointments.
- Clinical Errors: Wrong diagnoses, outdated medication lists, or false records of illnesses, resulting in inappropriate treatments or care denials.
- Systemic Impact: Healthwatch England noted that some patients missed diagnostic tests or were given unnecessary drugs, with errors severe enough to “put patients at risk,” according to CEO Louise Ansari.
The survey’s findings translate to millions of affected patients across England’s population, underscoring a pervasive issue within the NHS’s record-keeping processes.
Causes of Medical Record Errors
Several factors contribute to the high error rate, as identified by Healthwatch England and other analyses:
Inadequate IT Infrastructure: The NHS relies on a patchwork of digital systems, many of which are outdated or incompatible. A 2024 Guardian report highlighted safety risks in electronic health record rollouts, with one trust reporting 927 incidents after implementing new software. Incompatible systems can lead to data mismatches or incomplete records.
Workforce Pressures: High workloads and staff shortages exacerbate errors. NHS staff, often overstretched, may input data hastily or fail to update records. A 2025 Guardian article on NHS staff fatigue noted that exhaustion contributes to mistakes, such as mislabelling blood samples or incorrect documentation.
Poor Communication: Ineffective communication between departments or healthcare providers can result in fragmented records. For example, a GP’s records may not sync with hospital systems, leading to discrepancies. Healthwatch England cited this as a key contributor.
Bureaucratic Overload: Excessive administrative tasks divert time from accurate record-keeping. The Guardian reported that “high levels of unnecessary bureaucracy” strain NHS staff, increasing the likelihood of errors.
Consequences for Patients
The impact of these errors is profound:
- Care Delays or Denials: Patients with incorrect records may be refused necessary treatments or tests. For instance, a false diagnosis could lead to exclusion from eligibility for certain procedures.
- Inappropriate Treatments: Errors in medication history can result in patients receiving drugs they don’t need or missing critical prescriptions, posing health risks.
- Loss of Trust: The prevalence of errors erodes confidence in the NHS. A separate Healthwatch survey found 34% of patients distrust the NHS to use complaints to improve services, which may discourage reporting inaccuracies.
- Safety Risks: Serious errors, such as incorrect DNR orders, could lead to life-threatening outcomes, as highlighted by a patient’s experience.
Systemic Challenges in Addressing the Issue
The NHS faces significant hurdles in resolving these errors:
- Digital Transition: The Department of Health and Social Care acknowledged an “analogue NHS” and aims to digitise records, but rushed implementations risk further errors, as seen in past IT failures.
- Complaint Handling: Healthwatch England’s January 2025 report noted that only 9% of patients with poor care experiences complain, and over half are dissatisfied with the process, indicating a lack of accountability.
- Resource Constraints: Chronic underfunding and staffing shortages limit the NHS’s ability to invest in robust systems or training, perpetuating the cycle of errors.
What Can Patients Do?
Individuals can take proactive steps to mitigate the impact of medical record errors:
Review Your Records: Request access to your NHS medical records through your GP or hospital. In England, patients have a legal right to view their records under the Data Protection Act 2018. Check for inaccuracies in personal details, diagnoses, or treatments.
- How: Contact your GP practice or use the NHS App, which allows digital access to some records.
- Tip: Keep a personal log of appointments, medications, and diagnoses to cross-reference.
Report Errors Promptly: If you identify mistakes, inform your healthcare provider immediately. Healthwatch England encourages reporting to ensure corrections and improve care.
- How: Submit a written request to your GP or hospital, detailing the error. Follow up to confirm changes.
- Tip: Be specific (e.g., “My record lists a diabetes diagnosis, but I’ve never been diagnosed”).
Use Patient Advocacy Services: Healthwatch England and organisations like the Patients Association offer support for navigating complaints or correcting records.
- How: Contact one or more of the following, other advocacy groups are available:
- Healthwatch England (healthwatch.co.uk) or call their helpline.
- The Patients Association Free Helpline: 0800 345 7115
- NHS PALS (Patient Advice and Liaison Service) You can find PALS in your local hospital.
- Tip: Document all interactions for accountability.
Engage with the NHS Complaints Process: If errors lead to harm or dissatisfaction, file a formal complaint with the NHS provider or escalate to the Parliamentary and Health Service Ombudsman.
- How: Follow NHS guidance at nhs.uk. Complaints should be filed within 12 months of the incident.
- Tip: Reference the NHS Constitution, which guarantees accurate record-keeping.
Advocate for Systemic Change: Share experiences with Healthwatch England’s surveys or public campaigns to highlight the need for better IT systems and staff support.
- How: Participate in patient feedback forums or contact your local MP to raise awareness.
- Tip: Anonymised feedback can still drive policy changes.
Moving Forward: A Call for Reform
The revelation that one in four patients in England find errors in their medical records is a wake-up call for the NHS. While the government’s push for digitalisation is a step toward modernisation, it must be paired with robust training, interoperable systems, and adequate staffing. Healthwatch England’s Louise Ansari emphasised the need to “get the basics right,” a sentiment echoed by patients and advocates.
For now, patients must remain vigilant, proactively checking and correcting their records while advocating for systemic improvements. By combining individual action with collective pressure, there’s hope for a more accurate and reliable NHS record-keeping system, ensuring safer care for all. Though it does pose an other safeguarding issue for the upcoming Assisted Dying Bill!
Additional Sources
- The Guardian: “One in four patients in England find errors in medical records, watchdog says” (May 1, 2025). https://www.theguardian.com/society/2025/may/01/one-in-four-patients-in-england-find-errors-in-medical-records-watchdog-says
- England’s ‘complex’ health and care system harming patients, report says 10.05.2025 https://www.theguardian.com/society/2025/apr/10/englands-complex-health-and-care-system-harming-patients-report-says
- BBC News: Exhausted hospital staff putting patients at risk, says watchdog https://www.bbc.co.uk/news/articles/cd6jz3z7en6o
- BBC News: Repeated failures in reading scans costing lives, ombudsman says https://www.bbc.co.uk/news/articles/cdjykmlr2vwo
- Healthwatch England: Official blog on medical record inaccuracies (May 1, 2025). https://www.healthwatch.co.uk/have-your-say
- The Guardian: “NHS electronic health records pose ‘serious safety risks’” (September 22, 2024). https://www.theguardian.com/society/2024/sep/22/nhs-electronic-health-records-pose-serious-safety-risks
- The Guardian: “Quarter of people in England had poor NHS care in past year, report says” (January 27, 2025). https://www.theguardian.com/society/2025/jan/27/nhs-care-report-survey-healthwatch-england-complaints
- Posts on X from @HealthwatchE, @radionewshub, @dave43law (May 1–3, 2025). https://x.com/HealthwatchE/status/1918240342073041195
- BBC News: NHS computer issues linked to patient harm https://www.bbc.co.uk/news/articles/c4nn0vl2e78o
- Bullet-pointed Summary of Kim Leadbeater’s Terminally Ill Adults (End of Life) Bill & How to Oppose it: https://jenkteach.co.uk/bullet-pointed-summary-of-kim-leadbeaters-terminally-ill-adults-end-of-life-bill-how-to-oppose-it/
